Bladder Cancer
Overview
Bladder cancer is the sixth most common cancer in the United States. About 53,200 Americans are diagnosed with bladder cancer each year and 12.200 die annually of the disease. In recent decades there has been a steady increase in the incidence of bladder cancer. However, doctors are making progress in treatment and survival rates are improving.
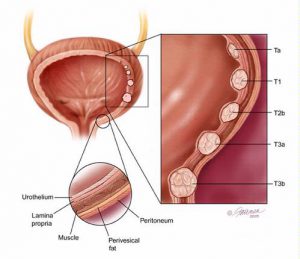
The bladder is a hollow balloon-shaped mostly muscular organ that stores urine until ready for release. The urine is produced in the kidneys. It flows through tubes called the ureters into the bladder and is discharged through the urethra during urination. The bladder muscle aids urination by contracting (tightening) to help force out the urine. A thin surface layer called the urothelium lines the inside of the bladder. Next is a layer of loose connective tissue called the lamina propia. Covering the lamina propia is the bladder muscle, covered on the outside by fat.
The ways in which bladder cancers develop and progess are only partly understood. However, a number of substances that cause the cancers to develop have been identified. Chief among them are cancer-causing agents in cigarette smoke and various industrial chemicals. Cigarette smoking alone has been estimated to cause 50 percent of all bladder cancer cases in the United States. Long-term workplace exposure to chemical compounds such as paints and solvents has been estimated to cause another 20 to 25 percent of bladder cancer cases. More than 90 percent of all bladder cancers originate in the urothelium. The majority of diagnosed bladder tumors are confined to the urothelium or the lamina propia and have not invaded the bladder muscle.
Symptoms
Painless blood in the urine (hematuria) is the most common symptom. It eventually occurs in nearly all cases of bladder cancer. In the majority of cases, the blood is visible during urination. In some cases, it is invisible except under a microsocope, and is usually discovered when analyzing a urine sample as part of a routine examination.
Hematuria does not by itself confirm the presence of bladder cancer. Blood in the urine has many possible causes. For example, it may result from a urinary tract infection or kidney stones rather than from cancer. It is important to note that hematuria, particularly microscopic, might be entirely normal for some individuals. A diagnostic investigation is necessary to determine whether bladder cancer is present.
Other symptoms of bladder cancer may include frequent urination and pain upon urination (dysuria).
Diagnosis
When bladder cancer is suspected, a comprehensive evaluation is performed including:
- Radiological Imaging – the kidneys, ureters and bladder are evaluated for signs of cancer (e.g. intravenous pyelogram or CT scan).
- Urine Cytology – the urine is examined under a microscope to look for cancer cells that may have been shed into the urine from the bladder lining.
- Cystoscopy – a procedure that allows direct viewing of the inside of the bladder. Cystoscopy is performed by inserting a viewing instrument called a cystoscope through the urethra and into the bladder. Looking through the cystoscope, the doctor is able to examine the bladder’s inner surfaces for signs of cancer. If tumors are present, their appearance, number, location and size are noted and the patient is scheduled to return for a surgical procedure to remove the tumor under general anesthesia or regional anesthesia.
- Transurethral Resection – a surgical procedure performed through the urethra to remove bladder tumors. The removed tisuue is submitted for pathologic examination.
- Tumor Marker Tests – the FDA has approved several tests that look for BTA or NMP22, proteins in the urine that may indicate cancer.
- Flourescence in Situ Hybridization (FISH) – a urine test that looks for chromosomal abnormalities and may provide early detection of transitional cell bladder cancer.
CANCER GRADING AND STAGING
If tissue is sampled and bladder cancer is found, the pathologist who examines the tissue will grade the tumor according to how much cells differ in appearance from normal cells. The most widely used grading systems classify tumors into three main grades; low, intermediate and high. The cells of low-grade tumors have minimal abnormalities. In high-grade tumors, the cells have become disorganized and many abnormalities are apparent. The grade indicates the tumor’s “aggression level” — how fast it is likely to grow and spread. High-grade tumors are the most agressive and the most likely to progress into the muscle of the bladder wall.
Staging of bladder cancers is based on how deeply a tumor has penetrated the bladder wall. The most commonly used system for staging bladder cancer is the TNM Systems developed by The American Joint Committee on Cancer.
Stages Ta and Tis (in the urothelium) and stage T1 (in the lamina propia) are the non-muscle invasive stages. Most Ta tumors are low grade, and most do not progress to invade the bladder muscle. Stage T1 tumors are much more likely to become muscle invasive. Stage Ta tumors often recur after treatment but they tend to recur with the same stage and grade.
The Tis stage classification is reserved for a type of high-grade cancer called carcinoma in situ (CIS). CIS usually appears through the cystoscope as a flat, reddish, velvety patch on the bladder lining. It is difficult to remove and is best treated with immunotherapy or chemotherapy. If untreated, CIS will likely progress to muscle-invasive disease.
Once your doctor has determined that you have bladder cancer, your doctor will determine what “stage” your cancer is in:
- Stage 1 – confined to the bladder lining; 60-70% of patients have Stage 1 disease
- Stage 2 – spread to the muscular walls of the bladder
- Stage 3 – spread to tissues around the bladder
- Stage 4 – spread to other organs
Treatments
Choosing an appropriate treatment for bladder cancer is a complex process and involves many factors the most important of which is tumor stage. The main types of treatment for bladder cancer are surgery, radiation therapy, immunotherapy and chemotherapy.
SURGERY
There are several kinds of surgery for bladder cancer. Some involve removing the tumor only while other involve removing the entire bladder. The type of surgery will depend on the stage of the cancer. The most common types of surgery include:
- Transurethral Resection – Transurethral Resection of the Bladder (TURBT) is the usual treatment method for patients who, when examined with a cystoscope, are found to have abnormal growths on the urothelium (stage Ta) and/or in the lamina propia (stage T1).
- Cystectomy – This surgery is used when the bladder cancer is invasive (stage T2, cancer that has spread into muscle layer of the bladder wall). It is necessary to cut through the abdomen. When only part of the bladder is removed, it is called a partial cystectomy. If the entire bladder is removed it is a radical cystectomy.
If the entire bladder is removed, nearby lymph nodes are also removed. In men, the prostate is removed as well. In women, the womb (uterus), ovaries, fallopian tubes, and a small part of the vagina are often removed as well.
When the entire bladder and nearby organs are removed, the risk of side effects are more seroius. Potential risks include bleeding, infection, urinary extravasation or obstruction. Also, another way to store and remove urine from the body is needed. Options include a urostomy or a continent diversion. For a urostomy, tissue taken from the small intestine (bowel) is attached to the ureters. A bag is worn outside the body to collect the urine.
Continent diversions do not require a bag outside the body. Instead, the surgeon will create a pouch from a small piece of intestine and attach it to the ureters. Urine is emptied when the person places a drainage tube into the hole of the diversion. Newer methods of surgery can route the urine into the urethra, making urination nearly normal.
Some problems from these methods could include wound infections, urine leaks, pouch stones and blockage of urine flow.
INTRAVESICAL CHEMOTHERAPY AND IMMUNOTHERAPY
Following removal, intravesical chemotherapy or intravesical immunotherapy may be used to try to prevent tumor recurrences. Intravesical means “within the bladder”. These therapeutic agents are put directly into the bladder through a catheter in the urethra, are retained for one to two hours and are then urinated out.
The chief intravesical agents currently available are thiotepa, doxorubicin, mitomycin C and bacillus Calmette-Guerin (BCG). The first three are drugs. The fourth, BCG, is a live but weakened vaccine strain of bovine tuberculosis. It was first used to immunize humans against tuberculosis. It is now one of the most effective agents for treating bladder cancer and especially for treating CIS.
Each of the four agents produces irritative side effects such as painful urination and the need to urinate frequently. In addition, BCG therapy carries a 24 percent risk of flu-like symptoms and a small risk (4 percent) of systemic infections. Thiotepa has a 13 percent risk of suppressing bone marrow activity causing a reduction in white blood cells and platelets.
CHEMOTHERAPY
Chemotherapy reffers to the use of drugs to kill cancer cells. Usually the drugs are given into a vein or by mouth. Once the drugs enter the bloodstream, they spread throughout the body. Chemotherapy is useful in treating cancer that has spread. While chemotherapy drugs kill cancer cells, they also damage some normal cells and this can lead to side effects. These side effects will depend on the type of drugs used, the amount taken, and the length of treatment. Temporary side effects might include nausea, vomiting, loss of appetite, hair loss, mouth sores, fatigue, and lethargy. Most of these side effects go away when treatment is over.
RADIATION THERAPY
Radiation therapy is treatment with high-energy rays (such as x-rays) to kill or shrink cancer cells. The radiation may come from outside the body or from radioactive materials placed directly in the tumor. After surgery, radiation can kill small deposits of cancer cells that may not be seen during surgery.
After transurethral surgery, giving radiation therapy and chemotherapy together is sometimes able to completely destroy cancers that would otherwise require cystectomy. If the tumor is in a position that makes surgery difficult, radiation may be used to shrink the tumor, making surgery easier. Radiation might also be used to ease the symptoms of advanced cancer. Mild skin irritation, nausea, bladder irritation, diarrhea, or fatigue may occur after radiation therapy. These problems usually go away when treatment ends.
Risk Factors
The following factors increase your risk of bladder cancer:
- Cigarette smoking – the single greatest risk factor
- Exposure to industrial chemicals
- Age – the average age is 67
- Sex – men are at much higher risk
- Race – Caucasians are at higher risk
- Family or personal history of bladder cancer
- Chronic bladder inflammation or foley catheter use
- Chemotherapy or radiation therapy for other cancers
- A high fat diet