Kidney Stones
Overview
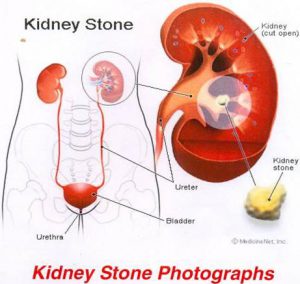
Kidney stones are among the most painful and prevalent of urologic disorders. Kidney stones typically form when your urine becomes too concentrated causing crystals to separate from the urine and build up inside the kidneys. Stones may be as small as a grain of sand or as large as a golfball. Some stones pass out of the body without the need for intervention, but others can cause severe pain if they become trapped in one of your ureters (the narrow tubes that carry urine from the kidneys to the bladder).
The urinary tract, or system, consists of the kidneys, ureters, bladder and urethra. The kidneys are two bean-shaped organs below the ribs in the back of the torso (area between ribs and hips). They are responsible for maintaining balance by removing extra water and wastes from the blood and converting to urine. The kidneys keep a stable balance of salts and other substances in the blood. They also produce hormones that build strong bones and help form red blood cells. Urine is carried by narrow muscular tubes, the ureters, from the kidneys to the bladder, a trainagular-shaped reservoir in the lower abdomen. Like a balloon, the bladder’s walls stretch and expand to store urine and then flatten when urine is emptied through the urethra to outside the body.
Symptoms
Usually, the symptom of a kidney stone is extreme pain that has been described as being worse than child labor pains. The pain often begins suddenly as the stone moves in the urinary tract, causing irritation and blockage. Typically, a person feels a sharp, cramping pain in the back and in the side of the area of the kidney or in the lower abdomen, which may spread to the groin. Also, sometimes a person will complain of blood in the urine, nausea and/or vomiting.
Occasionally stones do not produce any symptoms. But while they may be “silent,” they can be growing, even threatening irreversible damage to kidney function. More commonly, however, if a stone is not large enough to prompt major symptoms, it still can trigger a dull ache that is often confued with muscle or intestinal pain.
If the stone is too large to pass easily, pain continues as the muscles in the wall of the tiny ureter try to squeeze the stone along into the bladder. One may feel the need to urinate more often or feel a burning sensation during urination. In a man, pain may move down to the tip of the penis. If the stone is close to the lower end of the ureter at the opening into the bladder, a person will frequently feel like they have not fully completed urination.
Stones as small as 2 mm have caused many symptoms while those as large as a pea have quietly passed. If fever or chills accompany any of these symptoms, then there may be an infection. You should contact your urologist immediately.
Diagnosis
When a urinary stone is suspected, an immediate evaluation is required. Blood is obtained to check on overall kidney function as well as to exclude signs of infection throughout the body. Urine is sent for a urinalysis and culture. A simple x-ray of the abdomen is sometimes enough to pinpoint a calcification in the area of the kidneys or ureters, thus identifying a likely obstructing stone. If the x-ray does not provide enough information to make a diagnosis, then an intravenous pyelogram (IVP) may be performed. A kidney blocked by a stone will not be able to excrete the dye from the IVP test as quickly and may appear enlarged. A final diagnostic exam that can be done is an abdominal/pelvic CT scan, which is very sensitive and can detect almost all types of urinary stones.
Treatments
Stone size, the number of stones and their location are perhaps the most important factors in deciding the appropriate treatment for a patient with kidney stones. The composition of a stone, if known, can also affect the choice of treatments. Options for surgical treatment of stones include:
- Shock Wave Lithotripsy (SWL) – This is a completely non-invasive form of treatment in which an energy source generates a shock wave that is directed at a urinary stone within the kidney or ureter. Shock waves are transmitted to the patient either through a water bath, which the patient is placed in, or using a water-filled cushion that is placed against the skin. Ultrasound or fluoroscopy is used to locate the stone and focus the shock waves. The repeated force caused by the shock waves fragments the stone into small pieces.
SWL is most often performed under heavy sedation, although general anesthesia is sometimes used. Once the treatment is completed, the small stone particles then pass down the ureter and are eventually urinated away. In certain cases, a stent may need to be placed up the ureter just prior to SWL to assist in stone fragment passage.
Certain types of stone (cystine, calcium oxalate monohydrate) are resistant to SWL and usually require another treatment. In addition, larger stones (greater than 2.5 centimeters) may break into large pieces that can still block the kidney. Stones located in the lower portion of the kidney also have a decreased chance of passage. - Ureteroscopy (URS) – This treatment involves the use of a very small, fiber-optic instrument called a ureteroscope, which allows access to stones in the ureter or kidney. The ureteroscope allows your urologist to directly visualize the stone by progressing up the ureter via the bladder. No incisions are necessary but general anesthesia is used.
Once the stone is seen through the ureteroscope, a small basket-like device can be used to grasp smaller stones and remove them. If a stone is too large to remove, a laser, spark-generating probe or air-driven (pneumatic) probe can be passed through a channel built into the ureteroscope and the stone can be fragmented.
A straightforward case is complete once the stone has been shattered appropriately. However, if extensive manipulation was required to reach and/or treat the stone, your urologist may choose to place a stent within the ureter to allow the post-operative swelling to subside. - Percutaneous Nephrolithotomy (PNL) – PNL is the treatment of choice for large stones located within the kidney that will not be effectively treated with either SWL or URS. General anesthesia is required to perform a PNL. The main advantage of this approach compared to traditional open surgery is that only a small incision (about one centimeter) is required in the flank. The urologist then places a guide wire through the incision. The wire is inserted into the kidney under fluoroscopic guidance and directed down the ureter. A passage is then created around the wire using dilators to provide access into the kidney.
An instrument called a nephroscope is then passed into the kidney to visualize the stone. Fragmentation can then be done using an ultraonic probe or a laser. Because the tract allows passage of larger instruments, your urologist can suction out or grasp the stone fragments as they are produced. This results in a higher clearance of stone fragments than with SWL or URS.
Once the procedure is complete, a tube is left in the flank to drain the kidney for several days. - Open Surgery – A large incision is required in order to expose the kidney or portion of ureter that is involved with the stone. The portion of kidney overlying the stone or the ureteral wall is then surgically cut and the stone removed. At present, open surgery is used only for very complicated cases of stone disease.
Risk Factors
A stone forms in the kidney when there is an imbalance between certain urinary components — chemicals such as calcium, oxalate and phosphate — that promote crystallization and others that inhibit it.
Most common stones contain calcium in combination with oxalate and/or phosphate.
A less common type of stone is caused by infection in the urinary tract. This type of stone is called a struvite or infection stone. Much less common are the pure uric acid stones. Much rarer is the hereditary type of stones called cystine stones. Even more rare are those linked to hereditary disorders.
For unknown reasons, the number of people in the United States with kidney stones has been increasing over the past 20 years. Caucasians are more prone to develop kidney stones than African Americans. Although stones occur more frequently in men, the number of women who get them has been increasing over the past 10 years, causing the ratio to change. Kidney stones strike most typically between the ages of 20 and 40. If a person forms a stone, there is a 50 percent chance they will develop another stone.
A number of risk factors play major roles in stone formation. The first is loss of body fluids (dehydration). When one does not consume enough fluids during the day, the urine often becomes quite concentrated and darker. This increases the chance that crystals can form from materials within the urine, because there is less fluid available to dissolve them.
Diet can also affect probability of stone formation. A high-protein diet can cause the acid content in the body to increase. This decreases the amount of urinary citrate, a “good” chemical that helps prevent stones. As a result, stones are more likely to form. A high-salt diet is another risk factor, as an increased amount of sodium passing into the urine can also pull calcium along with it. The net result is an increased calcium level in the urine, which increases the probability for stones. Intake of oxalate-rich foods such as leafy green vegetables, tea or chocolate may also worsen the situation.
Finally, a family history of stones, especially in a first-degree relative (parent or sibling), dramatically increases the probability of having stones.
Scientists do not always know what makes stones form. While certain foods may promote stones in susceptible people, researchers do not believe that eating a specific item will cause stones in people who are not vulnerable. Yet they are confident that factors — such as a family or personal history or kidney stones and other urinary infections or diseases — have a definite connection to this problem. Climate and water intake may also play a role in stone formation.
Stones can also form because of obstruction to urinary passage like in prostate enlargement or stricture disease. Stone formation has also been linked to hyperparathyroidism, an endocrine disorder that results in more clacium in your urine. Susceptibility can also be raised if you are among the 70 percent of people with rare hereditary disorders such as cystinuria or primary hyperoxaluria who develop kidney stones because of excesses of the amino acid, cystine or the oxalate in your urine.
Another condition that can cause stones to form is absorptive hypercalciuria, surplus of calcium in the urine that occurs when the body absorbs too much from food. The high levels result in calcium oxalate or phosphate crystals forming in the kidneys or urinary tract. Similarly, hyperuricosuria, excess uric acid tied to gout or the excessive consumption of meat products, may also trigger kidney stones.
Consumption of calcium pills by a person who is at risk to form stones, certain diuretics or calcuim-based antacids may increase the risk of forming stones by increasing the amount of calcium in the urine. Calcium oxalate stones may also form in people who have chronic inflammation of the bowel or who have had an intestinal bypass operation or ostomy. This is because of loss of more water from the body as well as absorption of oxalate from the intestine.
Lifestyle Changes
More than half of those who develop one kidney stone will develop recurrent or additional stones. Your urologist may order special urine and blood tests to help determine how to decrease the risk of recurrence. Based upon these results your doctor may suggest you:
- Drink more water
- Reduce salt and/or protein intake
- Avoid foods high in oxalate
- Avoid/reduce caffeine
- Eat a special diet
- Take special medications or antibiotics
- Watch your calcium intake