Overview
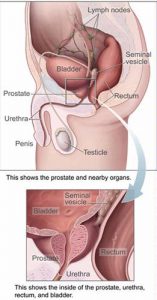
Prostatitis is an inflammation or infection of the prostate gland. It can affect men of any age. The most common urological problem in men aged 50 and older, prostatitis is not contagious and is not transmitted during sex. The prostate is a walnut-sized organ found only in men. Its main function is to produce semen, the fluid that carries sperm during ejaculation. Part of the male urinary system, it lies next to the bladder. Prostatitis often causes urinary symptoms because the prostate surrounds the urethra, the tube carrying urine out of the body.
The four types of prostatitis are:
- Chronic Pelvic Pain Syndrome (CPPS) – affects about 90% of men with prostatitis (Chronic Non-Bacterial Prostatitis)
- Asymptomatic Inflammatory Prostatitis – patients don’t have symptoms but their doctors find infection-fighting cells in the semen when checking for other problems such as prostate cancer or enlargement
- Acute Bacterial Prostatitis – the least common but easiest to treat
- Chronic Bacterial Prostatitis – also not common
Symptoms
The symptoms of the various prostatitis syndromes depends upon the category.
In acute bacterial prostatitis, the symptoms are severe and sudden and may cause the patient to seek emergency medical care. Chills, fever, severe burning during urination and the inability to completely empty the bladder are common.
In chronic bacterial prostatitis, the symptoms are similar but do not produce fever. They include: burning during urination; urinary frequency, especially at night; perineal, testicular, bladder and low back pain; and painful ejaculation. The condition can be episodic, with flare-ups and remissions, associated with infection, treatment and subsequent recurrence.
The symptoms of chronic prostatitis/chronic pelvic pain syndrome include difficult and sometimes painful urination, discomfort or pain in the perineum, bladder, testicles and penis as well as difficult and painful ejaculation. In some cases, these symptoms can be indistinguishable from those described above for chronic bacterial prostatitis.
Diagnosis
The correct diagnosis is very important because the treatment is different for the different types of prostatitis syndromes. In addition, it is extremely important to make sure that the symptoms are not caused by other conditions such as urethritis, cystitis, an enlarged prostate or cancer. To help make an accurate diagnosis, several types of examinations are useful.
To examine the prostate gland, the physician will perform a digital rectal examination (DRE). This is a simple examination in which the doctor will pass a lubricated, gloved finger into the rectum.
Because the prostate is located just in front of the rectum, it can be easily pressed. The physician will be able to determine whether the prostate is enlarged or tender. Lumps or firm areas can suggest the presence of prostate cancer. The physician wll also assess the degree of pain or discomfort the patient experiences as he presses the muscles and ligaments of the pelvic floor and perineum. If a man has prostatitis, the examination may produce momentary pain or discomfort but it causes neither damage nor significant prolonged pain.
If the physician requires a closer look at the prostate or decides that a biopsy is necessary, he may order a transrectal ultrasound, which allows him to visualize the prostate gland. If you are at risk for cancer, your physician will consider ordering a PSA test. During a prostate infection however, the PSA can be falsely elevated.
If your physician suspects that you have prostatitis or one of the other prostate problems, he may refer you to a urologist, a doctor who specializes in diseases of the urinary tract and male reproductive system, to confirm the diagnosis.
The urologist will repeat some of the examinations already performed by the first physician. The urologist will also assess the degree of pain or discomfort the patient experiences as he presses the prostate. The urologist may analyze various urine specimens as well as a specimen of prostatic fluid obtained by massaging the prostate gland during the DRE. The various urine specimens and prostatic fluid will be analyzed for signs of inflammation and infection. These samples may help the urologist determine whether your problem is inflammation or infection and whether the problem is in the urethra, bladder or prostate.
Other tests the urologist may consider employing include cystoscopy in which a small telescope is passed through the urethra into the bladder permitting examination of the urethra, prostate and bladder. The urologist may also order urine flow studies, which help measure the strength of your urine flow and any obstruction caused by the prostate, urethra or pelvic muscles.
Treatments
Your treatment depends on the type of prostatitis you have.
If acute bacterial prostatitis is diagnosed, the patient will need to take antibiotics for a minimum of 14 days. Sometimes, this means being admitted to the hospital and being given intravenous antibiotics. A catheter is sometimes required if the patient has difficulty urinating. Almost all acute infections can be cured with this treatment. Frequently, the antibiotics will be continued for as long as four weeks.
If chronic bacterial prostatitis is diagnosed, the patient will require antibiotics for a longer period of time, usually four to 12 weeks. About 75 percent of all cases of chronic bacterial prostatitis clear up with this treatment. Sometimes the symptoms recur and antibiotic therapy is again required.
For cases that do not respond to this treatment, long-term, low dose antibiotic therapy may be recommended to relieve the symptoms. Other medications (such as those used for nonbacterial prostatitis) or other treatments (e.g., prostate massage therapy) may also be used in difficult cases. In some rare cases, surgery on either the urethra or prostate may be recommended. There must be a specific anatomic problem, such as scar tissue in the urethra, for any surgery aimed at improving prostatitis to be effective.
The patient may not need antibiotics, if they are diagnosed with chronic pelvic pain syndrome. Frequently, physicians have difficulty trying to decide whether a patient has bacterial or non-bacterial prostatitis. This is because of the difficulties in obtaining a specimen and sometimes previous antibiotic therapy obscures the diagnosis. An organism that responds to antibiotics, but is difficult to diagnose may also cause chronic pelvic pain syndrome. For these reasons, antibiotics may be prescribed, at least initially, even when a definitive diagnosis of bacterial prostatitis has not been made with the appropriate tests. Your response to the antibiotic therapy will decide whether or not it should be continued. Many patients without a true infection may feel better during antibiotic therapy because many antibiotics have direct anti-inflammatory effects. Depending on your symptoms you may receive one of a variety of other treatments. These may consist of alpha-blockers, anti-inflammatory drugs, muscle relaxants, plant extracts (quercetin and/or bee pollen) and repetitive prostatic massage (to drain the prostate ducts).
Various heat therapies, biofeedback and relaxation exercises may alleviate some of the symptoms. You may be advised to discontinue some foods (e.g. spicy) and drinks (e.g. caffeinated, acidic) and avoid circumstances (e.g. bicycle riding) that exacerbate the problem.
Once a correct diagnosis has been made, one of the best therapies may be that of reassurance that the patient does not have a life threatening condition.
Treatment for asymptomatic prostatic inflammation is usually not required.