Effects of Commercially Available Soy Products on PSA in Androgen-deprivation-naïve and Castration-resistant Prostate Cancer
Abstract
Objective: No standard therapeutic option exists for men with prostate cancer who have failed local therapy, have no gross metastatic disease, and whose only manifestation of disease is a rising prostate-specific antigen (PSA) level. Soy products are able to affect PSA kinetics in some men with prostate cancer, and this effect has been attributed to the decreased expression of the androgen receptor and other mechanisms.
Methods: We treated 10 men with rising PSA levels after radical prostatectomy and salvage radiotherapy with commercially available soy products. Scans revealed no gross metastatic disease. Three men also had been receiving androgen-deprivation therapy (ADT) and had rising PSA levels that were consistent with castration-resistant (CR) disease. We reported the results of this modality on PSA levels, PSA kinetics, and the duration of PSA response.
Results: Responses occurred in 4 of 7 (57%) patients with ADT-naïve disease and 1 of 3 (33%) patients with CR disease. The median duration of treatment response was 24 months. The overall clinical benefit, therefore, was noted in 5 of 10 (50%) patients. Therapy was well tolerated.
Conclusions: Our findings are fairly congruent with what has been described in the literature on the use of this modality in prostate cancer. We used commercially available soy products. We also show that soy can provide benefit in CR prostate cancer. Our clinical experience suggests that soy supplementation using commercially available soy products can have durable beneficial effects on PSA levels and PSA kinetics in some men with prostate cancer.
Introduction
No standard therapeutic option exists for men with prostate cancer who have failed local therapy with radical prostatectomy (RP) and salvage radiotherapy (RT), have no gross metastatic disease, and whose only manifestation of disease is a rising prostate-specific antigen (PSA) level.[1] The therapeutic options for such patients include observation, androgen-deprivation therapy (ADT), or clinical trial.[1] The use of ADT in this scenario remains controversial because there is no proven survival benefit and treatment has potential morbidity, which may at a minimum impair the quality of life of these patients.[2] A nontoxic, inexpensive, readily available, and effective approach to this situation would be welcomed by patients and their caregivers.
Soybeans and their components have been studied extensively in prostate cancer research. A diet that is rich in soy has the potential to decrease the incidence of prostate cancer, and soy may modulate the disease process for established cancers.[3] In our clinical practice, we began to use commercially available soy milk as an alternative to observation in men with biochemical relapse of their prostate cancer. In addition, we have offered this therapy to select asymptomatic men with CR and low-volume disease as an initial treatment along with continued ADT in advance of the use of secondary hormonal manipulations and/or chemotherapy. We describe our experience in 10 men in clinical practice.
Patients and Methods
The clinical records of 10 men treated with soy products for biochemically relapsed prostate cancer (low but rising PSA levels) were reviewed. Three men also had been receiving maximum ADT and had rising PSA levels that were consistent with CR disease. These three patients continued on ADT while receiving soy products. Scans showed no gross metastatic disease. Assent to a trial of soy was obtained from each patient before starting them on soy products, and the information was documented in each patient’s clinical chart. The men were advised to drink 8-oz glasses of soy milk as the preferred soy source 3 times per day, but other sources of soy could be used if taken more than 3 times per day. Almost all of our patients consumed the same brand of soy milk (Silk, WhiteWave Foods, Broomfield, CO). Adherence was assessed by direct questioning during each clinic encounter and was documented in each patient’s medication history. For PSA kinetics to be derived, patients needed at least three PSA determinations per state of treatment, that is, presoy versus during soy. PSA kinetics (PSA velocity, PSA doubling time, and slope of PSA vs time curves) were calculated using the Memorial Sloan-Kettering Cancer Center PSA kinetics calculator. For PSA levels <0.1 ng/mL, a PSA level of 0.1 was assigned to allow calculation of the kinetics using the calculator. We also calculated the percentage of decline of PSA in responding patients by dividing the nadir PSA while receiving treatment with soy by the pretreatment PSA level, multiplying by 100, and subtracting from 100.
Results
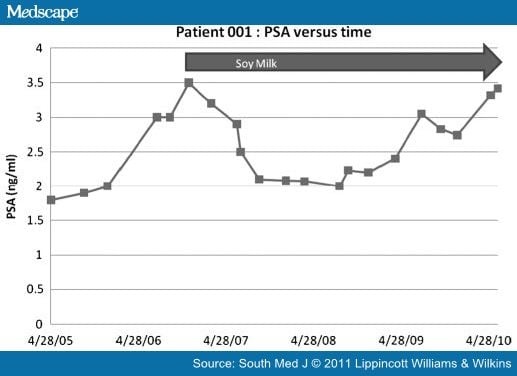
The complete results for each of these patients are summarized in the Table. Seven of the men were white, two were African American and one was Asian American. The median age was 61 years. None of the men had gross metastatic disease as determined by bone scan or computed tomography scan and all of them were asymptomatic. All 10 men had a biochemical relapse after both prior RP and RT; 3 of the men also had rising PSA levels postmedical ADT in addition to prior RP and RT that was consistent with CR disease. Of the 10 men, 9 drank commercially available soy milk and 1 man (patient 8) preferred to eat the equivalent in soy snacks instead. All of the men reported that they enjoyed consuming the soy products and were compliant because they did not consider this nutriceutical intervention to be burdensome. Five of the men had frank progression on soy milk. Three men had reductions in PSA and negative PSA kinetics. One man had an attenuated PSA response with a decrease in PSA velocity and doubling time. One man had stable PSA and PSA kinetics. Overall, clinical benefits (decrease, attenuation, and stability of PSA) were noted in 5 of 10 (50%) patients. The median duration of response was 24 months. The individual results of the PSA kinetics in 2 of these men, patients 1 and 4, are represented in Figs. 1 and 2. Both of these men had good responses to the soy in terms of absolute PSA levels and PSA kinetics for significant periods of time. Patient 1 had a transient response that lasted about 24 months followed by progression back to baseline on continued soy. Patient 2 continues to respond to soy milk.
Figure 1.
|
Figure 2. Prostate-specific antigen kinetics in patient 4. Patient 4 experienced a steady decline in PSA, which lasted approximately 3 years. |
Discussion
The present study was a retrospective observational study that evaluated the effect of commercially available soy products, mainly soy milk, on the PSA kinetics in a small group of men with both androgen-naïve and CR prostate cancer and biochemical relapse. We showed that 5 of 10 patients (50%) experienced a clinical benefit as manifested by decreased, attenuated, or stable PSA kinetics with soy product consumption. The other 5 patients (50%) showed frank progression of their disease. The results of our study suggest that some men with biochemical relapse of prostate cancer can benefit from soy consumption. Among the responders, 1 patient with CR prostate cancer showed a continuous decrease in PSA levels, which has persisted for more than 24 months. Gleason score and pathological features at the time of initial diagnosis did not show any significant correlation to the response to soy consumption, but the sample size was too small to comment on this aspect of the review. Our study, albeit a small retrospective analysis, is compelling because it was done in a real-world clinical practice using commercially available soy products. Our study was limited in its small sample size and being a retrospective single-arm review rather than a controlled study. We, therefore, did not measure any biochemical assays including isoflavone levels among this group of patients. Our data are congruent with the results published in the medical literature of the effect of soy products on PSA kinetics in men with similar states of prostate cancer. Uniquely, we show that this benefit may also extend to men with CR disease and that the benefit in some responders can be durable, lasting a median of 2 years.
The study of soy and its components on prostate cancer has a long history.[4] Soy appears to decrease the incidence of prostate cancer in men who consume it in large amounts. Soy products are the major source of isoflavonoids, which form one of the classes of phytoestrogens. There have been in vitro studies done examining the effect of phytoestrogens in prostate cancer cells. A group of scientists suggested that the use of low-dose genistein causes suppression of invasive growth through the reversal of epithelial mesenchymal transition in cancer cells, and this may justify using soy products as a chemopreventive approach for patients with prostate cancer.[5] The incidence of prostate cancer is lower in Asian countries than in Western populations, and this difference has been associated with the high soy content of the Asian diet.[6,7] Likewise, a diet high in soy seemed to lower the incidence of prostate cancer in a group of vegetarian Seventh-Day Adventist men.[8]
The mechanism for the effect of soy seems to be predominantly mediated through modulation of the interaction of androgens and the tumor receptor. Isoflavones are one class of compounds found in soy milk and in vitro they have been shown to act as cancer-preventive agents.[9] Isoflavones found in soy milk include genistein and daidzein. Genistein glycoside accounts for more than two-thirds of the total soybean isoflavone content[3,10] and has been shown to inhibit the growth of both androgen-dependent and androgen-independent prostate cancer cells in vitro.[11–13] The mechanism of action of genistein in preventing prostate cancer is still unclear, but it has been speculated that in addition to altering classic hormone receptor-mediated pathways, it acts by inhibiting the protein kinases and DNA topoisomerases and has an effect on apoptosis and angiogenesis.[14,15] In a prostate chemopreventive study in Lobound-Wistar rats, genistein demonstrated a dose-dependent decrease in the development of prostatic adenocarcinoma.[16] Daidzein is another component of the isoflavone class found in soy milk, which is thought to act by hormone manipulation. Another important component of soy milk is equol, which is produced by the bacterial conversion of daidzein in the intestine. It has a structure similar to estrogen and is supposed to interact via estrogen receptors.[17]
Steroid hormones control the growth of the prostate gland, and elevated levels of androgens have been linked with the risk of prostate cancer.[18,19] Androgen receptor (AR) expression also has been associated with the pathogenesis of prostate cancer. Both androgen action and the functional status of AR play an important role in the progression of prostate cancer. Lee demonstrated that increased AR expression was associated with lower recurrence-free survival and disease progression.[20] The consumption of isoflavone-rich proteins reduces AR expression in the prostate and eventually may help to prevent cancer.[21] Australian researchers found that men with early-stage prostate cancer who consumed a soy-enriched diet before RP had a statistically significant drop of 12.7% in PSA levels compared with the control group, whose PSA levels rose 40%.[22]
No standard treatment option exists for patients who have failed local therapy but do not have symptomatic gross metastatic disease. This would seem to be an ideal juncture to intervene with a low-toxicity nutriceutical therapy such as soy. Accordingly, in a phase II clinical trial of isoflavone use in patients with PSA recurrent prostate cancer after previous local therapy, it was shown that the slope of PSA versus time after study entry was significantly lower in 30% of the soy treatment group (6/20).[3] A double-blind, placebo-controlled crossover study showed that the consumption of a soy-based dietary supplement resulted in a significant decrease in the progression of PSA after potentially curative treatment.[23] The intake of a soy beverage daily for 6 months was demonstrated to be associated with a declining trend or more than double the prolongation of PSA doubling time in 41% of subjects.[24] Soy and its components had no effect on circulating hormone levels in men with prostate cancer, but they do downregulate AR expression.[5]
In our experience, 50% of patients experienced clinical benefit in their PSA levels, with 30% having prolonged reduction in absolute PSA levels. Our data are congruent with the response rates described in the studies mentioned above. For the first time, to the best of our knowledge, we show that response, if it occurs, can be prolonged, with a median duration of 24 months. Dietary modification with increased soy consumption may prove to be an important tool in prolonging “free” time before starting this group of patients on potentially more invasive cancer treatments. We and others also show that most men do not derive a measurable benefit from soy supplementation. Why some men respond and others do not and why some men develop resistance and others do not remains uncertain and requires further study to understand. It can be determined within several months of use whether soy is effective so that additional therapies can be considered. The effects of soy milk also may differ according to the stage of the disease.[25] One man with CR prostate cancer has continued to respond to soy snacks alone. This result emphasizes that being CR is not the same as being hormonally resistant.[26] In this case, the downgrade of AR expression induced by soy is analogous to secondary hormonal manipulation, as is frequently done in low-volume, asymptomatic CR prostate cancer.[27]
Further studies with larger defined patient populations will need to be conducted to understand the real benefit in this group of patients. More studies are needed that examine the effect of soy consumption on prostate cancer, PSA kinetics, and AR expression, and that correlative science assays may shed some light on the factors that may play a role in determining which patients with prostate cancer will respond to soy consumption as opposed to the nonresponders or patients who relapse after an initial response. In spite of the small sample size, our study supports that soy consumption may play a role in delaying PSA levels in some of the patients with prostate cancer who have failed prior local therapies such as surgery and/or radiotherapy. Another instance in which this modality may be of benefit is low-volume disease after initial ADT during intermittent ADT. Soy supplementation may delay the point of reinitiation of ADT, hence prolonging the time off ADT with an associated improvement in quality of life.
This article forms a purely descriptive report of our clinical practice and serves as a baseline for future clinical trials. Based on our experience, we are designing prospective clinical trials with associated laboratory studies to better understand this nutritional intervention in terms of mechanism of response, nonresponse, and resistance in these groups of men when the intervention is given long term.
Conclusions
Our clinical experience in 10 men with rising PSA levels after prior RP and RT suggests that treatment with commercially available soy products can have beneficial effects on PSA levels and PSA kinetics in some men. This effect can be sustained so that it could delay the need for ADT and/or other potentially morbid interventions. We observed that soy can benefit patients with CR prostate cancer. Our study was clearly limited in its sample size and its retrospective nature. Our study, like others of this modality, begs the question of why some men respond whereas others do not and why the response can be lost over time. Further study of this modality is needed because soy is an inexpensive, readily available, and well-tolerated means to delay the progression of prostate cancer, thus delaying the need for ADT or other potentially morbid treatments.